Opill’s FDA Approval: Implications for Pharmaceutical Regulation and Access to Care
By James René Jolin and Susannah Baruch
On July 13, 2023, the United States Food and Drug Administration (FDA) approved Opill (norgestrel) as the first daily oral contraceptive available for non-prescription use in the U.S. While the timeline for availability and price of Opill will ultimately be set by its manufacturer, Perrigo, this recent move represents a significant step forward in improving access to contraceptive health care. Indeed, shortly after Opill’s approval, the American College of Obstetricians and Gynecologists described the FDA’s decision as “a critically important advancement in the accessibility of reproductive health care.”
In response to this development, Petrie-Flom Center intern James René Jolin and Executive Director Susannah Baruch sat down to discuss its legal, regulatory, and public health implications. This interview has been edited for brevity and clarity.
James René Jolin (JRJ): This recent move by the FDA is one without precedent. From a legal and access to care perspective, what is its significance?
Susannah Baruch (SB): This decision, based on years of research and analysis, reflects the fact that there is a tremendous need for improved contraception access. For some people, this method and product will be the best way to get access, particularly for young people who need access to contraception and may prefer not to involve the formal medical system. Although there has been a great deal of conversation about this decision in relation to the Dobbs v. Jackson Women’s Health Organization (2022) case, it’s important to remember that this didn’t happen suddenly in response to Dobbs or anything else. For many years, there have been organizations and researchers and health care providers thinking this issue through, all before it came to the FDA. The process was careful, deliberate, and based in science, involving a great deal of sophisticated research. It was a long time coming.
JRJ: Can you give us a sense of what factors came into play in the decision?
SB: The FDA bases its decision-making on safety and efficacy, and considers risks and benefits. This product was determined to be safe, and it is expected to be more effective than currently available nonprescription contraceptive methods. At times during the process, FDA requested additional evidence from the manufacturer, to ensure they had the information they needed. Many observers expected that there would be more of a political fight around this issue but that wasn’t the case. The major medical groups supported it and view it as a real victory.
JRJ: You mentioned Dobbs earlier, which represented a kind of a marked shift in abortion jurisprudence in the United States and foretells potential legal battles that might arise over contraception — something about which I have written recently. What sort of legal challenges have already emerged or might emerge over this recent Opill approval, and how has Dobbs galvanized these challenges, if at all?
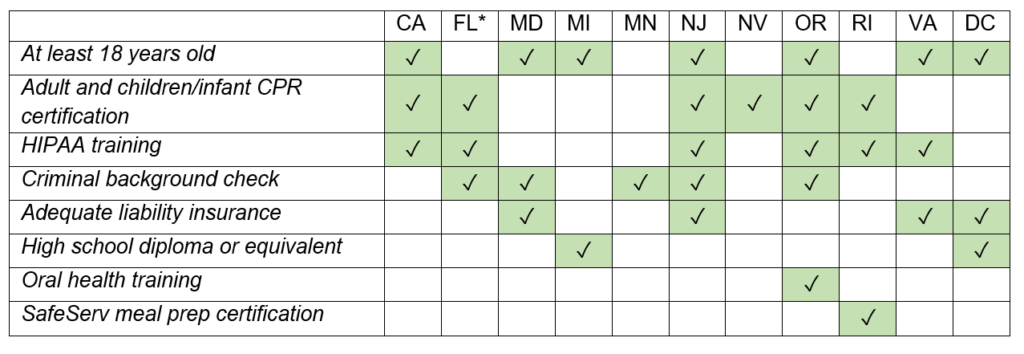
SB: Yes, there is often interest from people opposed to birth control in restricting it in one way or another. For example, minors’ access to contraception is a perennial issue. Recently there have been challenges in Texas to the rule that Title X-funded clinics, which provide contraception and other health care, cannot require parental consent. Title X is a federal program, and these are federally funded clinics, but the funding runs through the states.
So, we may see some challenges to the approval of new birth control methods or any other change that provides more access to contraception.
JRJ: The FDA, in its approval of Opill, essentially makes the argument that this will be a boon to access to contraceptive care. In your view, how much of a watershed moment do you think this recent approval of Opill is in ensuring equitable contraceptive access? Is there still more that needs to be done?
SB: It’s a big leap forward, and it’s not the end of the story. In our current system, nonprescription forms of birth control aren’t required to be covered by insurance. Access depends on cost, and advocacy groups are working to make Opill and other OTC methods much more accessible for all. My instinct is it’s going to be a huge change for many people, but some won’t be able to access it if it’s not covered by insurance.
JRJ: What are some potential steps governments might take on the state or federal level to ensure that people who don’t have insurance coverage can still access this form of care?
SB: Both Medicaid and the Title X program go a long way to making contraceptives available, and these same issues have to be worked out by those programs. Those decisions are made in the context of a complex system of federal and state law and regulations. Certainly, states and localities can help ensure over-the-counter methods are covered and available.
JRJ: Now, looking to the future of pharmaceutical regulation, the FDA approval of Opill is a significant milestone, from a legal or regulatory perspective. Do you think that this recent approval changes the calculus for future drug approvals or regulations of the pharmaceutical industry, or for people seeking this form of care?
SB: There was a time when health care providers thought that it was important to require women to go to the OBGYN in order to get a contraceptive prescription. The thinking was that it was a way to ensure people are linked to the health care system: come in once a year, and we will do a general checkup before you can get your prescription. Then health care providers saw that the benefits of giving access to contraceptives without that hurdle outweighed the theoretical benefits of forcing them to come in for a checkup.
In my view, we are seeing willingness by both patients and providers to color outside the lines to get care, to think beyond the most traditional ways of people getting their health care. At Petrie-Flom, we are thinking about this trend and what it means for health care in the future. For example, the home is a new arena for health care, from home tests for COVID-19, to in-home monitoring of cardiac symptoms, to self-managed abortion, to medical marijuana. People want to take care of their health, and giving them tools they need can improve access, which is critical. People deserve to be trusted to make these decisions for themselves and we should have systems that provide access to expertise and care in case people have questions or something goes wrong.
JRJ: My last question recognizes that we are coming up on an election year, in which there may be a change of party in power. How likely is it in your view that this recent move by the FDA will outlast the Biden administration? How durable are these kinds of approvals?
SB: It’s hard to make predictions. My sense watching the policy discussions for decades is that for access to contraception, there’s less likely to be push back. Contraception is close to a universally accessed form of health care. Taking away access is not a political battle too many people want to fight. Certainly, the current legal challenge to the original FDA approval of mifepristone decades ago seems like a reaction to Dobbs, as we know mifepristone used with misoprostol is an increasingly popular way for people to self-manage their abortion. If I had to predict, I would not expect a similar attack on Opill, but that doesn’t mean there won’t be more discussions about appropriate access to contraception, in general.